Ready to transform your health?
Unlock access to expert guidance and a weight care plan crafted just for you.
What is HRT for Menopause? Benefits & Risks
Hormone replacement therapy explained: benefits, risks, and timing. Learn how HRT treats menopause symptoms and protects long-term health

Table of Contents
Table of Contents
Understanding Menopause and What It Does to Your Body
What Is Hormone Replacement Therapy (HRT)?
Types of HRT
Not All Hormones Are Equal
How You Take It
The Critical Role of Timing: When You Start Matters
Benefits of HRT
Eliminates Hot Flashes and Night Sweats
Supports Brain Function and Mood
Protects Your Heart
Preserves Bone Strength
May Improve Blood Sugar Control
Treats Vaginal and Sexual Problems
Risks of HRT
Breast Cancer Risk
Heart Disease and Timing
Blood Clots and Stroke
Autoimmune Disease
Who Should Consider HRT?
Who Should Avoid HRT?
Making Your Decision
The Bottom Line
Understanding Menopause and What It Does to Your Body
What Is Hormone Replacement Therapy (HRT)?
Types of HRT
Not All Hormones Are Equal
How You Take It
The Critical Role of Timing: When You Start Matters
Benefits of HRT
Eliminates Hot Flashes and Night Sweats
Supports Brain Function and Mood
Protects Your Heart
Preserves Bone Strength
May Improve Blood Sugar Control
Treats Vaginal and Sexual Problems
Risks of HRT
Breast Cancer Risk
Heart Disease and Timing
Blood Clots and Stroke
Autoimmune Disease
Who Should Consider HRT?
Who Should Avoid HRT?
Making Your Decision
The Bottom Line
Menopause is a natural life change that happens to every woman. But the symptoms can range from a minor annoyance to truly difficult problems. If hot flashes wake you up at night, mood changes hurt your relationships, or brain fog makes work harder, you're not alone, and there are proven solutions that can help.
Hormone replacement therapy (HRT), also called menopausal hormone therapy (MHT), is the most effective treatment for menopause symptoms. But with so much confusing information online and worries about safety, many women don't know if HRT is right for them.
This guide will help explain what HRT is, how it works, and its benefits and risks.
Understanding Menopause and What It Does to Your Body
Menopause is a natural transition that actually begins four to six years before your last period, during a phase called perimenopause. During this time, your hormone levels fluctuate dramatically as your body produces less estrogen.
Common symptoms include:
Hot flushes and night sweats
Sleep problems and insomnia
Mood changes, anxiety, and depression
"Brain fog" and memory issues
Vaginal dryness and painful sex
Decreased interest in sex
Bone loss
Metabolic changes that raise your risk for heart disease and diabetes
Every woman's experience differs based on factors like age at menopause, overall health, environment, and culture. Some women barely notice the transition, while others have symptoms severe enough to affect their work, relationships, and mental health.
What Is Hormone Replacement Therapy (HRT)?
Hormone replacement therapy supplements the hormones your body stops producing after menopause. While estrogen is the primary hormone replaced, the exact treatment depends on your individual needs.
Types of HRT
Estrogen-Only Therapy: For women who had their uterus removed (hysterectomy), estrogen alone is sufficient since there's no uterine lining to protect.
Combined Estrogen-Progesterone Therapy: Women with an intact uterus need both estrogen and progesterone (or progestin). Without progesterone to balance estrogen's effects, the uterine lining thickens excessively, raising cancer risk.
Not All Hormones Are Equal
Research shows important differences between hormone types. Estradiol, which is bioidentical to your body's natural estrogen, has a better safety profile than conjugated equine estrogens, with lower risks for blood clots and metabolic issues.
The progesterone type also matters. Studies suggest micronized progesterone and dydrogesterone may carry lower breast cancer risk than synthetic progestins, though more research is needed to confirm this.
How You Take It
Pills: Convenient but processed through your liver first.
Skin patches or gels: Bypass liver metabolism, potentially reducing blood clot and stroke risk compared to oral forms.
Vaginal creams/tablets: Ideal for localized urogenital symptoms with minimal systemic absorption.
Newer options: Estetrol selectively activates estrogen receptors while minimizing liver effects.
The Critical Role of Timing: When You Start Matters
One of the most important discoveries in menopause medicine is that timing dramatically affects both benefits and risks.
Research on the "timing hypothesis" shows that starting HRT closer to menopause provides cardiovascular and brain health benefits not seen with later initiation. This finding revolutionized medical thinking about HRT and explains contradictory results from older studies.
For women who start HRT before age 60 or within 10 years of menopause, the therapy significantly reduces death from all causes and cardiovascular disease. These are benefits that even cholesterol medications can't match. The key is vessel health: healthy blood vessels respond positively to estrogen, while diseased vessels may react negatively.
Benefits of HRT
Eliminates Hot Flashes and Night Sweats
HRT remains unmatched for treating vasomotor symptoms. Studies consistently show it eliminates or substantially reduces hot flashes and night sweats in most women, leading to better sleep and daily functioning.
Supports Brain Function and Mood
Research highlights that neurological symptoms like sleep disturbance, brain fog, and mood changes significantly impact quality of life, work productivity, and physical health during the menopausal transition. The relationship between estrogen and cognitive function is complex but crucial for many women experiencing mental fatigue, difficulty concentrating, or memory lapses.
Protects Your Heart
Perhaps the most compelling reason to consider HRT is its cardiovascular benefit, but only when initiated at the right time. According to research, HRT effects depend on timing of initiation, age, underlying tissue health, and treatment duration.
Starting early provides substantial protection against heart disease and reduces overall mortality. Starting late (more than 10 years post-menopause) offers no such benefits and may increase certain risks.
The Long-Term Survival Benefit
Research tracking over 1,000 women for nearly two decades provides clear evidence of HRT's mortality benefit. The graph below shows cumulative survival probability over 18 years, comparing women who used HRT versus those who didn't:
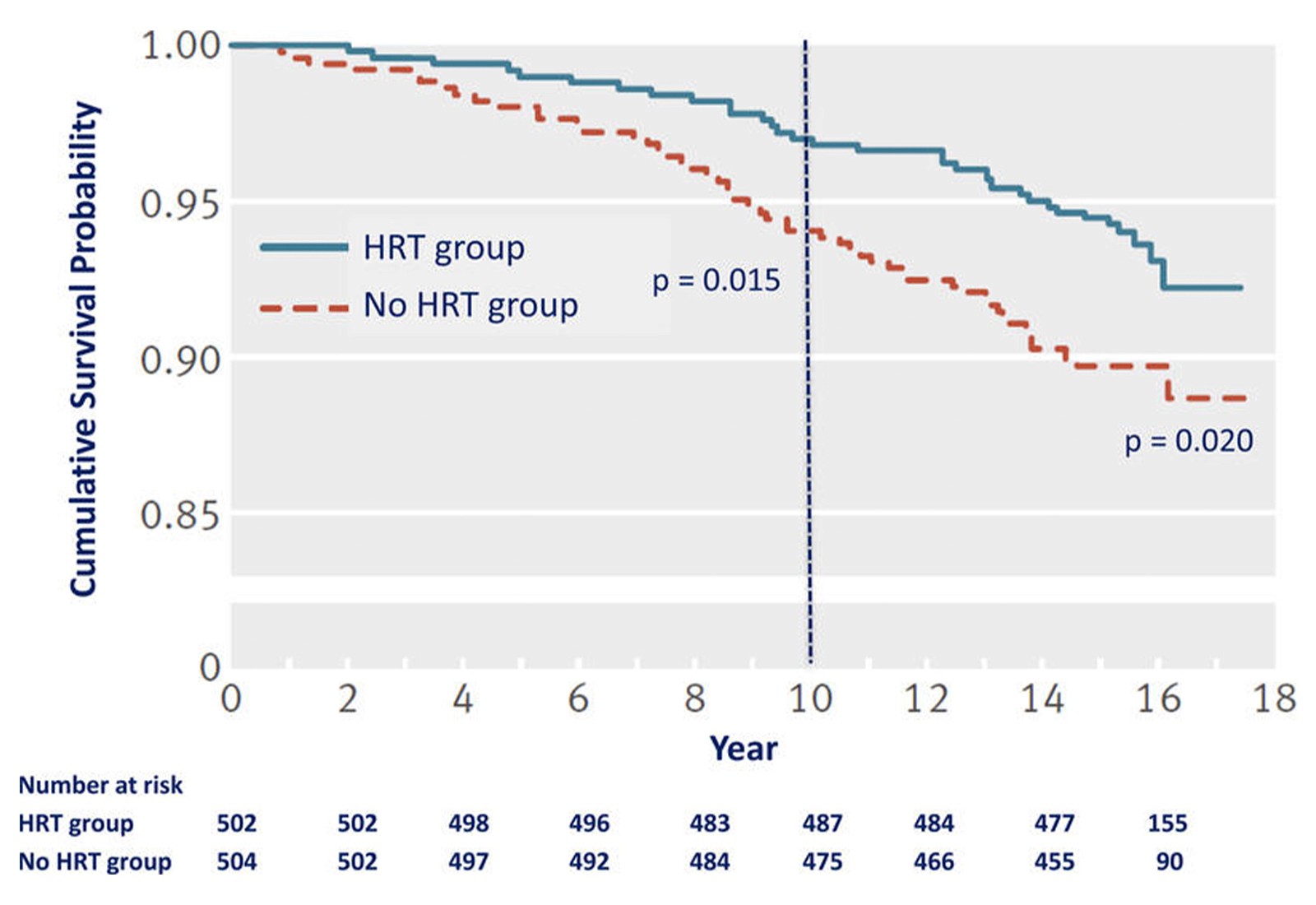
Figure adapted from Hodis HN, Mack WJ. Cancer Journal. 2022;28(3):208-223. This survival curve from the Danish Osteoporosis Study shows a statistically significant reduction of cardiovascular disease by 52% after 10 years of randomized hormone replacement therapy relative to no HRT, and reduction by 39% after 16 years of total follow-up.
What this graph shows: The blue line represents women using HRT, while the red dashed line represents women not using HRT. Higher lines mean better survival rates. The separation between the lines demonstrates that women using HRT had consistently better survival throughout the study period. The vertical dashed line at year 10 marks an important milestone, and the p-values (0.015 and 0.020) indicate these differences are statistically significant, not due to chance.
Preserves Bone Strength
Estrogen deficiency at menopause accelerates bone loss, increasing fracture risk. HRT effectively prevents this bone loss and reduces fractures, particularly in the spine and hip. These are injuries that can dramatically impact quality of life in older age.
May Improve Blood Sugar Control
Evidence suggests HRT can affect glucose control in women with diabetes and may influence diabetes risk in those without the condition. However, experts emphasize that HRT shouldn't be used solely for diabetes prevention. For women with existing diabetes, treatment decisions should be individualized based on age, metabolic status, and cardiovascular risk factors.
Treats Vaginal and Sexual Problems
Vaginal dryness, painful intercourse, and urinary symptoms seriously affect many postmenopausal women's sexual health and quality of life. Low-dose vaginal estrogen is the first-line treatment for these urogenital symptoms, with excellent effectiveness and minimal absorption into the bloodstream. Estriol, a weaker estrogen form, has gained recognition for safely and effectively treating genitourinary symptoms.
Risks of HRT
While people often exaggerate HRT risks, understanding actual risks helps you make informed decisions. All treatment options carry specific benefits and risks that vary by individual situation.
Breast Cancer Risk
This remains the primary concern for most women considering HRT, though the relationship is nuanced:
Estrogen-only therapy (for women post-hysterectomy) appears to carry lower breast cancer risk than combined therapy
Combined therapy risk varies with your baseline risk and specific treatment type
Progesterone type matters: Micronized progesterone and dydrogesterone show lower associated risk than synthetic progestins in observational studies
Experts recommend evaluating your baseline breast cancer risk before starting HRT and learning about modifiable risk factors that decrease risk regardless of hormone use.
Importantly, HRT-associated risks including breast cancer, stroke, and blood clots are rare; fewer than 10 events per 10,000 women, which is comparable to risks from other common medications.
Heart Disease and Timing
As emphasized earlier, cardiovascular effects depend critically on when you start. Early initiation (before 60 or within 10 years of menopause) reduces heart disease risk. Late initiation provides no benefit and may increase risk.
Blood Clots and Stroke
Blood clot risk remains rare (fewer than 10 events per 10,000 women) and can be further reduced by choosing transdermal forms (patches/gels) over pills, which bypass liver processing.
Similarly, transdermal preparations appear less likely to increase stroke risk compared to oral forms.
Autoimmune Disease
Recent research found modest associations between HRT and rheumatoid arthritis. Current users showed an 18% higher risk compared to non-users, with long-term use (4+ years) showing 19% higher risk. However, the absolute increase remains small. Women with autoimmune susceptibility should discuss individual risk-benefit ratios with their healthcare provider.
Who Should Consider HRT?
HRT may be appropriate for women who:
Have moderate to severe symptoms affecting quality of life
Are younger than 60 or within 10 years of menopause
Have no contraindications
Understand benefits and risks and prefer hormone treatment
Who Should Avoid HRT?
You should not use HRT if you have:
Estrogen-dependent cancers
History of blood clots, stroke, or cardiovascular disease
Active liver disease
Unexplained vaginal bleeding
Known or suspected pregnancy
Women with these conditions should explore alternatives with their healthcare provider.
Making Your Decision
As one major review emphasizes, decisions about menopause therapy should be personalized, considering your symptoms, health status, risk profile, life expectations, and treatment availability and cost.
Your decision should factor in:
How symptoms affect your quality of life
Your age and time since menopause
Personal and family medical history
Baseline cardiovascular and breast cancer risk
Your preferences and values
Healthcare providers and patients can use the extensive HRT research to make informed decisions about symptom management, disease prevention, and mortality reduction—keeping in mind that prevention strategies must be personalized.
The Bottom Line
Research demonstrates that HRT is a sex-specific, time-dependent therapy that reduces all-cause mortality and aging-related diseases when started appropriately, with an excellent risk profile for eligible women.
Women spend roughly 40% of their lives in menopause, and symptoms can substantially impair quality of life. You deserve to live those decades feeling your best, with effective symptom management and optimized long-term health.
The key is working with a knowledgeable healthcare provider who can assess your individual situation, discuss options thoroughly, and support you in making the choice that fits your health profile, symptom severity, and personal values.
If you're experiencing menopause symptoms, consider connecting with a healthcare provider through Mochi Health to discuss whether hormone therapy might be right for you. Check your eligibility here
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider before starting, stopping, or changing any medication or treatment plan.
References
Cobin RH, Goodman NF; AACE Reproductive Endocrinology Scientific Committee. AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS AND AMERICAN COLLEGE OF ENDOCRINOLOGY POSITION STATEMENT ON MENOPAUSE-2017 UPDATE. Endocrine Practice. 2017;23(7):869-880. doi:10.4158/EP171828.PS | PubMed
Davis SR, Lambrinoudaki I, Lumsden M, et al. Menopause. Nature Reviews Disease Primers. 2015;1:15004. doi:10.1038/nrdp.2015.4 | PubMed
Gava G, Orsili I, Alvisi S, et al. Cognition, Mood and Sleep in Menopausal Transition: The Role of Menopause Hormone Therapy. Medicina (Kaunas). 2019;55(10):668. doi:10.3390/medicina55100668 | PubMed
Gompel A, Simcock R. Menopausal hormone treatment and breast cancer. Lancet Diabetes & Endocrinology. 2026 Jan 28:S2213-8587(25)00394-8. doi:10.1016/S2213-8587(25)00394-8 | PubMed
Guimarães C, Balbinot E, Marçal F, et al. Hormone therapy in menopause increases rheumatoid arthritis risk: A systematic review and meta-analysis. Seminars in Arthritis and Rheumatism. 2026;77:152935. doi:10.1016/j.semarthrit.2026.152935 | PubMed
Hodis HN, Mack WJ. Menopausal Hormone Replacement Therapy and Reduction of All-Cause Mortality and Cardiovascular Disease: It Is About Time and Timing. Cancer Journal. 2022;28(3):208-223. doi:10.1097/PPO.0000000000000591 | PubMed
Soltani A, Voedisch AJ. A review of estrogens used in menopausal hormone therapy. Current Opinion in Obstetrics & Gynecology. 2026 Feb 2. doi:10.1097/GCO.0000000000001090 | PubMed
Stuenkel CA. Menopause, hormone therapy and diabetes. Climacteric. 2017;20(1):11-21. doi:10.1080/13697137.2016.1267723 | PubMed
Menopause is a natural life change that happens to every woman. But the symptoms can range from a minor annoyance to truly difficult problems. If hot flashes wake you up at night, mood changes hurt your relationships, or brain fog makes work harder, you're not alone, and there are proven solutions that can help.
Hormone replacement therapy (HRT), also called menopausal hormone therapy (MHT), is the most effective treatment for menopause symptoms. But with so much confusing information online and worries about safety, many women don't know if HRT is right for them.
This guide will help explain what HRT is, how it works, and its benefits and risks.
Understanding Menopause and What It Does to Your Body
Menopause is a natural transition that actually begins four to six years before your last period, during a phase called perimenopause. During this time, your hormone levels fluctuate dramatically as your body produces less estrogen.
Common symptoms include:
Hot flushes and night sweats
Sleep problems and insomnia
Mood changes, anxiety, and depression
"Brain fog" and memory issues
Vaginal dryness and painful sex
Decreased interest in sex
Bone loss
Metabolic changes that raise your risk for heart disease and diabetes
Every woman's experience differs based on factors like age at menopause, overall health, environment, and culture. Some women barely notice the transition, while others have symptoms severe enough to affect their work, relationships, and mental health.
What Is Hormone Replacement Therapy (HRT)?
Hormone replacement therapy supplements the hormones your body stops producing after menopause. While estrogen is the primary hormone replaced, the exact treatment depends on your individual needs.
Types of HRT
Estrogen-Only Therapy: For women who had their uterus removed (hysterectomy), estrogen alone is sufficient since there's no uterine lining to protect.
Combined Estrogen-Progesterone Therapy: Women with an intact uterus need both estrogen and progesterone (or progestin). Without progesterone to balance estrogen's effects, the uterine lining thickens excessively, raising cancer risk.
Not All Hormones Are Equal
Research shows important differences between hormone types. Estradiol, which is bioidentical to your body's natural estrogen, has a better safety profile than conjugated equine estrogens, with lower risks for blood clots and metabolic issues.
The progesterone type also matters. Studies suggest micronized progesterone and dydrogesterone may carry lower breast cancer risk than synthetic progestins, though more research is needed to confirm this.
How You Take It
Pills: Convenient but processed through your liver first.
Skin patches or gels: Bypass liver metabolism, potentially reducing blood clot and stroke risk compared to oral forms.
Vaginal creams/tablets: Ideal for localized urogenital symptoms with minimal systemic absorption.
Newer options: Estetrol selectively activates estrogen receptors while minimizing liver effects.
The Critical Role of Timing: When You Start Matters
One of the most important discoveries in menopause medicine is that timing dramatically affects both benefits and risks.
Research on the "timing hypothesis" shows that starting HRT closer to menopause provides cardiovascular and brain health benefits not seen with later initiation. This finding revolutionized medical thinking about HRT and explains contradictory results from older studies.
For women who start HRT before age 60 or within 10 years of menopause, the therapy significantly reduces death from all causes and cardiovascular disease. These are benefits that even cholesterol medications can't match. The key is vessel health: healthy blood vessels respond positively to estrogen, while diseased vessels may react negatively.
Benefits of HRT
Eliminates Hot Flashes and Night Sweats
HRT remains unmatched for treating vasomotor symptoms. Studies consistently show it eliminates or substantially reduces hot flashes and night sweats in most women, leading to better sleep and daily functioning.
Supports Brain Function and Mood
Research highlights that neurological symptoms like sleep disturbance, brain fog, and mood changes significantly impact quality of life, work productivity, and physical health during the menopausal transition. The relationship between estrogen and cognitive function is complex but crucial for many women experiencing mental fatigue, difficulty concentrating, or memory lapses.
Protects Your Heart
Perhaps the most compelling reason to consider HRT is its cardiovascular benefit, but only when initiated at the right time. According to research, HRT effects depend on timing of initiation, age, underlying tissue health, and treatment duration.
Starting early provides substantial protection against heart disease and reduces overall mortality. Starting late (more than 10 years post-menopause) offers no such benefits and may increase certain risks.
The Long-Term Survival Benefit
Research tracking over 1,000 women for nearly two decades provides clear evidence of HRT's mortality benefit. The graph below shows cumulative survival probability over 18 years, comparing women who used HRT versus those who didn't:
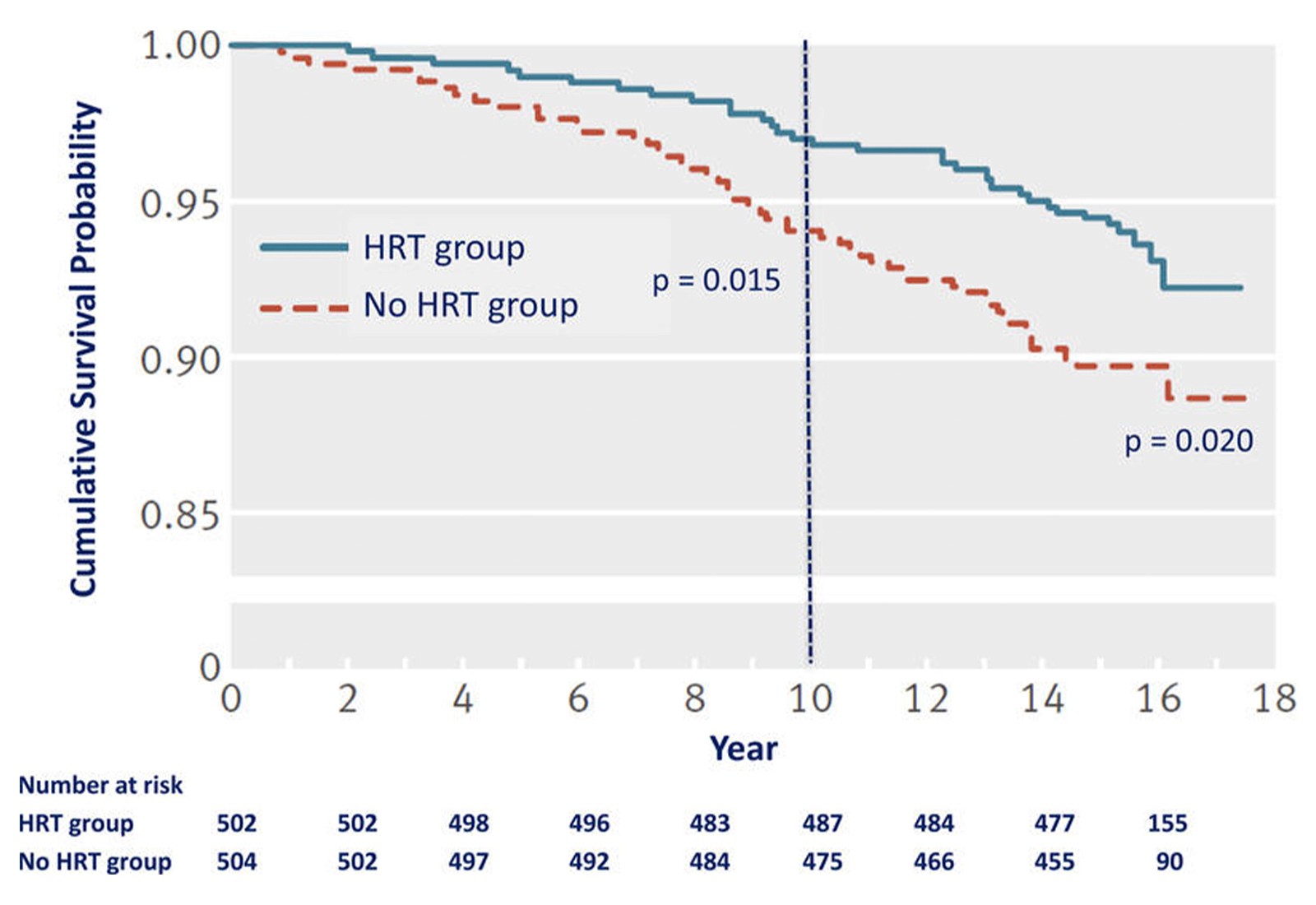
Figure adapted from Hodis HN, Mack WJ. Cancer Journal. 2022;28(3):208-223. This survival curve from the Danish Osteoporosis Study shows a statistically significant reduction of cardiovascular disease by 52% after 10 years of randomized hormone replacement therapy relative to no HRT, and reduction by 39% after 16 years of total follow-up.
What this graph shows: The blue line represents women using HRT, while the red dashed line represents women not using HRT. Higher lines mean better survival rates. The separation between the lines demonstrates that women using HRT had consistently better survival throughout the study period. The vertical dashed line at year 10 marks an important milestone, and the p-values (0.015 and 0.020) indicate these differences are statistically significant, not due to chance.
Preserves Bone Strength
Estrogen deficiency at menopause accelerates bone loss, increasing fracture risk. HRT effectively prevents this bone loss and reduces fractures, particularly in the spine and hip. These are injuries that can dramatically impact quality of life in older age.
May Improve Blood Sugar Control
Evidence suggests HRT can affect glucose control in women with diabetes and may influence diabetes risk in those without the condition. However, experts emphasize that HRT shouldn't be used solely for diabetes prevention. For women with existing diabetes, treatment decisions should be individualized based on age, metabolic status, and cardiovascular risk factors.
Treats Vaginal and Sexual Problems
Vaginal dryness, painful intercourse, and urinary symptoms seriously affect many postmenopausal women's sexual health and quality of life. Low-dose vaginal estrogen is the first-line treatment for these urogenital symptoms, with excellent effectiveness and minimal absorption into the bloodstream. Estriol, a weaker estrogen form, has gained recognition for safely and effectively treating genitourinary symptoms.
Risks of HRT
While people often exaggerate HRT risks, understanding actual risks helps you make informed decisions. All treatment options carry specific benefits and risks that vary by individual situation.
Breast Cancer Risk
This remains the primary concern for most women considering HRT, though the relationship is nuanced:
Estrogen-only therapy (for women post-hysterectomy) appears to carry lower breast cancer risk than combined therapy
Combined therapy risk varies with your baseline risk and specific treatment type
Progesterone type matters: Micronized progesterone and dydrogesterone show lower associated risk than synthetic progestins in observational studies
Experts recommend evaluating your baseline breast cancer risk before starting HRT and learning about modifiable risk factors that decrease risk regardless of hormone use.
Importantly, HRT-associated risks including breast cancer, stroke, and blood clots are rare; fewer than 10 events per 10,000 women, which is comparable to risks from other common medications.
Heart Disease and Timing
As emphasized earlier, cardiovascular effects depend critically on when you start. Early initiation (before 60 or within 10 years of menopause) reduces heart disease risk. Late initiation provides no benefit and may increase risk.
Blood Clots and Stroke
Blood clot risk remains rare (fewer than 10 events per 10,000 women) and can be further reduced by choosing transdermal forms (patches/gels) over pills, which bypass liver processing.
Similarly, transdermal preparations appear less likely to increase stroke risk compared to oral forms.
Autoimmune Disease
Recent research found modest associations between HRT and rheumatoid arthritis. Current users showed an 18% higher risk compared to non-users, with long-term use (4+ years) showing 19% higher risk. However, the absolute increase remains small. Women with autoimmune susceptibility should discuss individual risk-benefit ratios with their healthcare provider.
Who Should Consider HRT?
HRT may be appropriate for women who:
Have moderate to severe symptoms affecting quality of life
Are younger than 60 or within 10 years of menopause
Have no contraindications
Understand benefits and risks and prefer hormone treatment
Who Should Avoid HRT?
You should not use HRT if you have:
Estrogen-dependent cancers
History of blood clots, stroke, or cardiovascular disease
Active liver disease
Unexplained vaginal bleeding
Known or suspected pregnancy
Women with these conditions should explore alternatives with their healthcare provider.
Making Your Decision
As one major review emphasizes, decisions about menopause therapy should be personalized, considering your symptoms, health status, risk profile, life expectations, and treatment availability and cost.
Your decision should factor in:
How symptoms affect your quality of life
Your age and time since menopause
Personal and family medical history
Baseline cardiovascular and breast cancer risk
Your preferences and values
Healthcare providers and patients can use the extensive HRT research to make informed decisions about symptom management, disease prevention, and mortality reduction—keeping in mind that prevention strategies must be personalized.
The Bottom Line
Research demonstrates that HRT is a sex-specific, time-dependent therapy that reduces all-cause mortality and aging-related diseases when started appropriately, with an excellent risk profile for eligible women.
Women spend roughly 40% of their lives in menopause, and symptoms can substantially impair quality of life. You deserve to live those decades feeling your best, with effective symptom management and optimized long-term health.
The key is working with a knowledgeable healthcare provider who can assess your individual situation, discuss options thoroughly, and support you in making the choice that fits your health profile, symptom severity, and personal values.
If you're experiencing menopause symptoms, consider connecting with a healthcare provider through Mochi Health to discuss whether hormone therapy might be right for you. Check your eligibility here
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider before starting, stopping, or changing any medication or treatment plan.
References
Cobin RH, Goodman NF; AACE Reproductive Endocrinology Scientific Committee. AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS AND AMERICAN COLLEGE OF ENDOCRINOLOGY POSITION STATEMENT ON MENOPAUSE-2017 UPDATE. Endocrine Practice. 2017;23(7):869-880. doi:10.4158/EP171828.PS | PubMed
Davis SR, Lambrinoudaki I, Lumsden M, et al. Menopause. Nature Reviews Disease Primers. 2015;1:15004. doi:10.1038/nrdp.2015.4 | PubMed
Gava G, Orsili I, Alvisi S, et al. Cognition, Mood and Sleep in Menopausal Transition: The Role of Menopause Hormone Therapy. Medicina (Kaunas). 2019;55(10):668. doi:10.3390/medicina55100668 | PubMed
Gompel A, Simcock R. Menopausal hormone treatment and breast cancer. Lancet Diabetes & Endocrinology. 2026 Jan 28:S2213-8587(25)00394-8. doi:10.1016/S2213-8587(25)00394-8 | PubMed
Guimarães C, Balbinot E, Marçal F, et al. Hormone therapy in menopause increases rheumatoid arthritis risk: A systematic review and meta-analysis. Seminars in Arthritis and Rheumatism. 2026;77:152935. doi:10.1016/j.semarthrit.2026.152935 | PubMed
Hodis HN, Mack WJ. Menopausal Hormone Replacement Therapy and Reduction of All-Cause Mortality and Cardiovascular Disease: It Is About Time and Timing. Cancer Journal. 2022;28(3):208-223. doi:10.1097/PPO.0000000000000591 | PubMed
Soltani A, Voedisch AJ. A review of estrogens used in menopausal hormone therapy. Current Opinion in Obstetrics & Gynecology. 2026 Feb 2. doi:10.1097/GCO.0000000000001090 | PubMed
Stuenkel CA. Menopause, hormone therapy and diabetes. Climacteric. 2017;20(1):11-21. doi:10.1080/13697137.2016.1267723 | PubMed
Read next
Ready to transform your health?
Unlock access to expert guidance and a weight care plan crafted just for you.

Ready to transform your health?
Unlock access to expert guidance and a weight care plan crafted just for you.

Ready to transform your health?
Unlock access to expert guidance and a weight care plan crafted just for you.


© 2026 Mochi Health
All professional medical services are provided by licensed physicians and clinicians affiliated with independently owned and operated professional practices. Mochi Health Corp. provides administrative and technology services to affiliated medical practices it supports, and does not provide any professional medical services itself.


© 2026 Mochi Health
All professional medical services are provided by licensed physicians and clinicians affiliated with independently owned and operated professional practices. Mochi Health Corp. provides administrative and technology services to affiliated medical practices it supports, and does not provide any professional medical services itself.


© 2026 Mochi Health
All professional medical services are provided by licensed physicians and clinicians affiliated with independently owned and operated professional practices. Mochi Health Corp. provides administrative and technology services to affiliated medical practices it supports, and does not provide any professional medical services itself.



















