Ready to transform your health?
Unlock access to expert guidance and a weight care plan crafted just for you.
Ready to transform your health?
Unlock access to expert guidance and a weight care plan crafted just for you.
Similar Articles
Similar Articles


Is Zofran Safe with Semaglutide? What You Need to Know
Is Zofran Safe with Semaglutide? What You Need to Know


Does Semaglutide Cause Headaches? What You Should Know
Does Semaglutide Cause Headaches? What You Should Know
CBL-514: A New Injectable Approach to Targeted Fat Reduction
CBL-514: A New Injectable Approach to Targeted Fat Reduction
GLP-1s for Hyperinsulinemia: How Lowering Insulin Can Trigger Weight Loss
GLP-1s for Hyperinsulinemia: How Lowering Insulin Can Trigger Weight Loss
GLP-1s for Hyperinsulinemia: How Lowering Insulin Can Trigger Weight Loss
Hyperinsulinemia makes weight loss extremely difficult. Learn how GLP 1 medications help lower insulin levels, improve metabolic health, decrease cravings, and support sustainable weight loss.
Hyperinsulinemia makes weight loss extremely difficult. Learn how GLP 1 medications help lower insulin levels, improve metabolic health, decrease cravings, and support sustainable weight loss.
Hyperinsulinemia makes weight loss extremely difficult. Learn how GLP 1 medications help lower insulin levels, improve metabolic health, decrease cravings, and support sustainable weight loss.



Table of Contents
Table of Contents
Table of Contents
What Hyperinsulinemia Is and Why It Matters
How Hyperinsulinemia Affects Weight
How GLP-1 Medications Lower Insulin Levels
Why Lowering Insulin Supports Weight Loss
What Studies Show About GLP-1s and Insulin Levels
How Symptoms Change When Insulin Improves
Who Benefits Most From GLP-1 Treatment
How Lifestyle Interacts With GLP-1 Treatment
What Symptoms Require Attention
FAQs
References
What Hyperinsulinemia Is and Why It Matters
How Hyperinsulinemia Affects Weight
How GLP-1 Medications Lower Insulin Levels
Why Lowering Insulin Supports Weight Loss
What Studies Show About GLP-1s and Insulin Levels
How Symptoms Change When Insulin Improves
Who Benefits Most From GLP-1 Treatment
How Lifestyle Interacts With GLP-1 Treatment
What Symptoms Require Attention
FAQs
References
What Hyperinsulinemia Is and Why It Matters
How Hyperinsulinemia Affects Weight
How GLP-1 Medications Lower Insulin Levels
Why Lowering Insulin Supports Weight Loss
What Studies Show About GLP-1s and Insulin Levels
How Symptoms Change When Insulin Improves
Who Benefits Most From GLP-1 Treatment
How Lifestyle Interacts With GLP-1 Treatment
What Symptoms Require Attention
FAQs
References
Hyperinsulinemia is one of the most overlooked drivers of weight gain and metabolic challenges. It is a condition where the body produces too much insulin, often for years, long before blood sugar becomes elevated. High insulin levels increase hunger, promote fat storage, and make it unusually hard to lose weight even with strict dieting or exercise. Many people live with hyperinsulinemia without knowing it, because routine blood tests do not check insulin directly.
GLP 1 medications such as semaglutide and tirzepatide have become powerful tools for treating obesity and insulin resistance. One of the most important reasons they work so well for people with hyperinsulinemia is that they help the body reduce unnecessary insulin production. When insulin levels fall, appetite becomes calmer, blood sugar becomes more stable, cravings decrease, and the metabolism begins to shift away from constant fat storage.
This article explains what hyperinsulinemia is, how it develops, how GLP 1s lower insulin, and why this creates an ideal environment for weight loss. You will also learn how symptoms change once insulin stabilizes, what clinical studies show, and how to know if this approach may be right for you.
If you want to know whether GLP 1 treatment fits your metabolism and health goals, you can check your eligibility here.
What Hyperinsulinemia Is and Why It Matters
Hyperinsulinemia means that the pancreas is producing more insulin than the body needs. Insulin is a hormone that allows the body to use or store energy from food. When insulin is high, the body shifts into storage mode. It becomes difficult to burn fat for energy, hunger signals intensify, and cravings increase.
People with hyperinsulinemia often describe feeling hungry shortly after meals, feeling shaky between meals, or craving carbohydrates more intensely. Over time the body becomes less responsive to insulin, a condition known as insulin resistance. To compensate, the pancreas produces even more insulin, creating a cycle that makes weight loss extremely difficult.

How Hyperinsulinemia Affects Weight
High insulin levels directly influence weight through several pathways. Insulin increases hunger by stimulating ghrelin, the hormone that drives appetite. It also reduces the body’s ability to burn fat for fuel, which makes calorie deficits feel more draining. People with hyperinsulinemia often describe hitting weight loss plateaus early or gaining weight back very quickly after dieting.
The body’s constant insulin production also raises inflammation, increases water retention, and can cause rapid swings in blood sugar that lead to cravings, irritability, or fatigue. These swings can make healthy eating feel harder than it should be.
This is why many people feel like they are fighting their biology rather than simply their habits. Hyperinsulinemia makes the appetite louder and the metabolism slower. GLP-1 medications help reverse this.
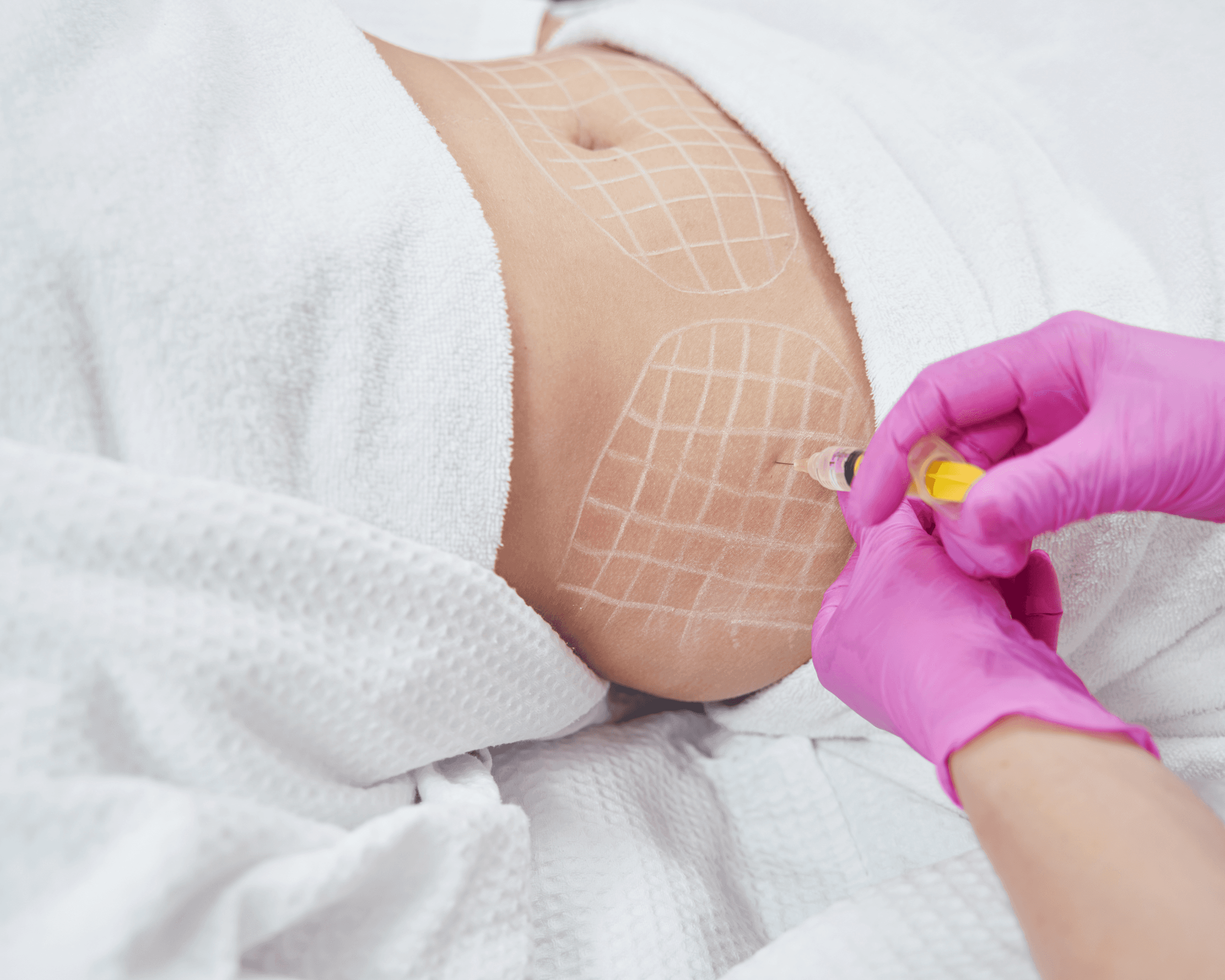
How GLP-1 Medications Lower Insulin Levels
GLP-1 medications reduce insulin secretion in a controlled and natural way. They do not shut insulin off. Instead, they help the body release insulin only when appropriate and at more stable levels. This makes blood sugar steadier and reduces the large insulin bursts that drive hunger and fat storage.
Semaglutide, tirzepatide, and other GLP 1s work by slowing digestion, calming appetite hormones, stabilizing glucose, and reducing the spikes that trigger excessive insulin release. Over time this helps the pancreas rest and reduces the hormonal noise that drives overeating. As researchers look to refine this process even further, new non-peptide medications like orforglipron are being developed to target these same metabolic pathways in a convenient daily pill.
Why Lowering Insulin Supports Weight Loss
When insulin levels fall, the body stops storing energy constantly and begins burning stored fat more efficiently. Appetite becomes quieter. Cravings lessen. People feel satisfied with smaller meals. Blood sugar stays steady rather than crashing. The combination reduces the emotional and physical drivers of overeating.
Lower insulin also improves resting metabolic rate. Research shows that people who reduce insulin levels early in weight loss maintain more lean mass and experience fewer weight loss plateaus because their metabolic adaptation is less severe. This means the body does not panic or slow down as dramatically when calories decrease.
Most importantly, when insulin resistance improves, the body becomes more flexible in how it uses energy. This flexibility makes long term weight maintenance more achievable.
What Studies Show About GLP-1s and Insulin Levels
Several studies demonstrate that GLP 1 medications significantly improve insulin resistance, hyperinsulinemia, and overall metabolic health.
A 2021 semaglutide study published in The Lancet followed people with obesity and elevated insulin levels. Participants saw large reductions in fasting insulin, improved HOMA IR (a measure of insulin resistance), and meaningful weight loss. People with the highest baseline insulin levels often experienced the greatest improvements.
Another trial evaluating tirzepatide found even stronger reductions in insulin and C peptide levels. Participants showed improved glucose control, better insulin sensitivity, and substantial reductions in visceral fat. Visceral fat is strongly linked with hyperinsulinemia, so this reduction is a key part of long term metabolic improvement.
A third study in metabolic syndrome demonstrated that lowering insulin levels resulted in significant improvements in inflammation markers and liver function. Given the link between hyperinsulinemia and fatty liver disease, this is a notable benefit.
Together, these studies show that GLP 1s do more than reduce appetite. They actively reshape the metabolic environment that makes weight loss difficult in the first place.
How Symptoms Change When Insulin Improves
People with hyperinsulinemia often feel the effects of GLP 1 treatment quickly. Many describe fewer cravings, more stable energy, and a sense of calmness around food. Others notice they can go longer between meals without feeling shaky or irritable. Afternoon fatigue often improves.
Appetite becomes predictable instead of chaotic. People notice they feel satisfied without large portions. The emotional drive to eat decreases because the hormonal pressure behind those urges weakens.
These changes reflect a deeper improvement in insulin sensitivity. When the body is no longer fighting against high insulin, weight loss feels more natural and sustainable.
Who Benefits Most From GLP-1 Treatment
GLP 1 medications may be especially helpful for people who have symptoms of hyperinsulinemia such as fatigue after meals, intense carb cravings, difficulty losing weight, weight gain around the abdomen, irregular blood sugar swings, or family history of type 2 diabetes.
People with PCOS, metabolic syndrome, or insulin resistant obesity often respond particularly well because GLP 1s target the core hormonal pathways involved in their symptoms.
Anyone who has tried dieting repeatedly without success, despite eating well and exercising, may also benefit. Often the barrier is hormonal, not behavioral.
If you want to see whether your symptoms match hyperinsulinemia or insulin resistance, you can start by checking your eligibility here.
How Lifestyle Interacts With GLP-1 Treatment
Lowering insulin through GLP 1 therapy works best when paired with steady protein intake, high fiber foods, hydration, and gentle movement. These choices further support insulin sensitivity and help preserve muscle mass. Strength training and balanced meals contribute to long term metabolic health and reduce weight regain risk.
As GLP 1 therapy reduces cravings, many people find it easier to make food choices that align with their goals. This creates a self reinforcing cycle where improved appetite control supports better nutrition, which supports better insulin sensitivity, which supports easier weight loss.
What Symptoms Require Attention
Most insulin related improvements feel positive. However, if blood sugar becomes too low, symptoms like dizziness, shakiness, or sweating can occur. This is rare in people without diabetes but should be evaluated if it happens. Persistent nausea, constipation, or intense fullness may also require dose adjustments.
Severe or persistent abdominal pain, vomiting, or inability to tolerate fluids should be discussed with a clinician. These symptoms are uncommon but require evaluation.
FAQs
Does high insulin make it harder to lose weight?
Yes. High insulin drives fat storage and increases hunger, which makes weight loss difficult.
Do GLP 1s lower insulin?
GLP 1s reduce excessive insulin release and improve insulin sensitivity.
How fast do insulin levels improve?
Many people see improvements within the first eight to twelve weeks.
Can I have hyperinsulinemia with normal blood sugar?
Yes. High insulin often appears years before high glucose.
Do GLP 1s cure hyperinsulinemia?
They help reduce insulin resistance, but long term outcomes depend on lifestyle and metabolic health.
Check Your Eligibility
If you want to learn whether GLP 1 treatment or compounded semaglutide is an option for your hyperinsulinemia, cravings, or metabolic symptoms, you can begin with Mochi’s eligibility questionnaire. It takes only a few minutes and provides personalized guidance based on your health history and goals. Check your eligibility here.
References
Jastreboff, A. M., et al. (2022). Tirzepatide once weekly for the treatment of obesity. New England Journal of Medicine, 387, 205 to 216.
Kahal, H., et al. (2021). Hyperinsulinemia and metabolic disease. Diabetologia, 64, 994 to 1007.
Lundgren, J. R., et al. (2021). Healthy weight loss maintenance with semaglutide. The Lancet, 397, 971 to 984.
Meier, J. J. (2020). GLP 1 receptor agonists and insulin dynamics. Journal of Endocrinology, 246, R57 to R75.
Sanyal, A. J., et al. (2019). Insulin resistance, NASH, and metabolic syndrome. Hepatology, 70, 137 to 149.
Thomas, D. D., Corkey, B. E., Istfan, N. W., & Apovian, C. M. (2019). Hyperinsulinemia: An early indicator of metabolic dysfunction. Journal of the Endocrine Society, 3(9), 1727 to 1747. https://doi.org/10.1210/js.2019-00065
Hyperinsulinemia is one of the most overlooked drivers of weight gain and metabolic challenges. It is a condition where the body produces too much insulin, often for years, long before blood sugar becomes elevated. High insulin levels increase hunger, promote fat storage, and make it unusually hard to lose weight even with strict dieting or exercise. Many people live with hyperinsulinemia without knowing it, because routine blood tests do not check insulin directly.
GLP 1 medications such as semaglutide and tirzepatide have become powerful tools for treating obesity and insulin resistance. One of the most important reasons they work so well for people with hyperinsulinemia is that they help the body reduce unnecessary insulin production. When insulin levels fall, appetite becomes calmer, blood sugar becomes more stable, cravings decrease, and the metabolism begins to shift away from constant fat storage.
This article explains what hyperinsulinemia is, how it develops, how GLP 1s lower insulin, and why this creates an ideal environment for weight loss. You will also learn how symptoms change once insulin stabilizes, what clinical studies show, and how to know if this approach may be right for you.
If you want to know whether GLP 1 treatment fits your metabolism and health goals, you can check your eligibility here.
What Hyperinsulinemia Is and Why It Matters
Hyperinsulinemia means that the pancreas is producing more insulin than the body needs. Insulin is a hormone that allows the body to use or store energy from food. When insulin is high, the body shifts into storage mode. It becomes difficult to burn fat for energy, hunger signals intensify, and cravings increase.
People with hyperinsulinemia often describe feeling hungry shortly after meals, feeling shaky between meals, or craving carbohydrates more intensely. Over time the body becomes less responsive to insulin, a condition known as insulin resistance. To compensate, the pancreas produces even more insulin, creating a cycle that makes weight loss extremely difficult.

How Hyperinsulinemia Affects Weight
High insulin levels directly influence weight through several pathways. Insulin increases hunger by stimulating ghrelin, the hormone that drives appetite. It also reduces the body’s ability to burn fat for fuel, which makes calorie deficits feel more draining. People with hyperinsulinemia often describe hitting weight loss plateaus early or gaining weight back very quickly after dieting.
The body’s constant insulin production also raises inflammation, increases water retention, and can cause rapid swings in blood sugar that lead to cravings, irritability, or fatigue. These swings can make healthy eating feel harder than it should be.
This is why many people feel like they are fighting their biology rather than simply their habits. Hyperinsulinemia makes the appetite louder and the metabolism slower. GLP-1 medications help reverse this.
How GLP-1 Medications Lower Insulin Levels
GLP-1 medications reduce insulin secretion in a controlled and natural way. They do not shut insulin off. Instead, they help the body release insulin only when appropriate and at more stable levels. This makes blood sugar steadier and reduces the large insulin bursts that drive hunger and fat storage.
Semaglutide, tirzepatide, and other GLP 1s work by slowing digestion, calming appetite hormones, stabilizing glucose, and reducing the spikes that trigger excessive insulin release. Over time this helps the pancreas rest and reduces the hormonal noise that drives overeating. As researchers look to refine this process even further, new non-peptide medications like orforglipron are being developed to target these same metabolic pathways in a convenient daily pill.
Why Lowering Insulin Supports Weight Loss
When insulin levels fall, the body stops storing energy constantly and begins burning stored fat more efficiently. Appetite becomes quieter. Cravings lessen. People feel satisfied with smaller meals. Blood sugar stays steady rather than crashing. The combination reduces the emotional and physical drivers of overeating.
Lower insulin also improves resting metabolic rate. Research shows that people who reduce insulin levels early in weight loss maintain more lean mass and experience fewer weight loss plateaus because their metabolic adaptation is less severe. This means the body does not panic or slow down as dramatically when calories decrease.
Most importantly, when insulin resistance improves, the body becomes more flexible in how it uses energy. This flexibility makes long term weight maintenance more achievable.
What Studies Show About GLP-1s and Insulin Levels
Several studies demonstrate that GLP 1 medications significantly improve insulin resistance, hyperinsulinemia, and overall metabolic health.
A 2021 semaglutide study published in The Lancet followed people with obesity and elevated insulin levels. Participants saw large reductions in fasting insulin, improved HOMA IR (a measure of insulin resistance), and meaningful weight loss. People with the highest baseline insulin levels often experienced the greatest improvements.
Another trial evaluating tirzepatide found even stronger reductions in insulin and C peptide levels. Participants showed improved glucose control, better insulin sensitivity, and substantial reductions in visceral fat. Visceral fat is strongly linked with hyperinsulinemia, so this reduction is a key part of long term metabolic improvement.
A third study in metabolic syndrome demonstrated that lowering insulin levels resulted in significant improvements in inflammation markers and liver function. Given the link between hyperinsulinemia and fatty liver disease, this is a notable benefit.
Together, these studies show that GLP 1s do more than reduce appetite. They actively reshape the metabolic environment that makes weight loss difficult in the first place.
How Symptoms Change When Insulin Improves
People with hyperinsulinemia often feel the effects of GLP 1 treatment quickly. Many describe fewer cravings, more stable energy, and a sense of calmness around food. Others notice they can go longer between meals without feeling shaky or irritable. Afternoon fatigue often improves.
Appetite becomes predictable instead of chaotic. People notice they feel satisfied without large portions. The emotional drive to eat decreases because the hormonal pressure behind those urges weakens.
These changes reflect a deeper improvement in insulin sensitivity. When the body is no longer fighting against high insulin, weight loss feels more natural and sustainable.
Who Benefits Most From GLP-1 Treatment
GLP 1 medications may be especially helpful for people who have symptoms of hyperinsulinemia such as fatigue after meals, intense carb cravings, difficulty losing weight, weight gain around the abdomen, irregular blood sugar swings, or family history of type 2 diabetes.
People with PCOS, metabolic syndrome, or insulin resistant obesity often respond particularly well because GLP 1s target the core hormonal pathways involved in their symptoms.
Anyone who has tried dieting repeatedly without success, despite eating well and exercising, may also benefit. Often the barrier is hormonal, not behavioral.
If you want to see whether your symptoms match hyperinsulinemia or insulin resistance, you can start by checking your eligibility here.
How Lifestyle Interacts With GLP-1 Treatment
Lowering insulin through GLP 1 therapy works best when paired with steady protein intake, high fiber foods, hydration, and gentle movement. These choices further support insulin sensitivity and help preserve muscle mass. Strength training and balanced meals contribute to long term metabolic health and reduce weight regain risk.
As GLP 1 therapy reduces cravings, many people find it easier to make food choices that align with their goals. This creates a self reinforcing cycle where improved appetite control supports better nutrition, which supports better insulin sensitivity, which supports easier weight loss.
What Symptoms Require Attention
Most insulin related improvements feel positive. However, if blood sugar becomes too low, symptoms like dizziness, shakiness, or sweating can occur. This is rare in people without diabetes but should be evaluated if it happens. Persistent nausea, constipation, or intense fullness may also require dose adjustments.
Severe or persistent abdominal pain, vomiting, or inability to tolerate fluids should be discussed with a clinician. These symptoms are uncommon but require evaluation.
FAQs
Does high insulin make it harder to lose weight?
Yes. High insulin drives fat storage and increases hunger, which makes weight loss difficult.
Do GLP 1s lower insulin?
GLP 1s reduce excessive insulin release and improve insulin sensitivity.
How fast do insulin levels improve?
Many people see improvements within the first eight to twelve weeks.
Can I have hyperinsulinemia with normal blood sugar?
Yes. High insulin often appears years before high glucose.
Do GLP 1s cure hyperinsulinemia?
They help reduce insulin resistance, but long term outcomes depend on lifestyle and metabolic health.
Check Your Eligibility
If you want to learn whether GLP 1 treatment or compounded semaglutide is an option for your hyperinsulinemia, cravings, or metabolic symptoms, you can begin with Mochi’s eligibility questionnaire. It takes only a few minutes and provides personalized guidance based on your health history and goals. Check your eligibility here.
References
Jastreboff, A. M., et al. (2022). Tirzepatide once weekly for the treatment of obesity. New England Journal of Medicine, 387, 205 to 216.
Kahal, H., et al. (2021). Hyperinsulinemia and metabolic disease. Diabetologia, 64, 994 to 1007.
Lundgren, J. R., et al. (2021). Healthy weight loss maintenance with semaglutide. The Lancet, 397, 971 to 984.
Meier, J. J. (2020). GLP 1 receptor agonists and insulin dynamics. Journal of Endocrinology, 246, R57 to R75.
Sanyal, A. J., et al. (2019). Insulin resistance, NASH, and metabolic syndrome. Hepatology, 70, 137 to 149.
Thomas, D. D., Corkey, B. E., Istfan, N. W., & Apovian, C. M. (2019). Hyperinsulinemia: An early indicator of metabolic dysfunction. Journal of the Endocrine Society, 3(9), 1727 to 1747. https://doi.org/10.1210/js.2019-00065
Hyperinsulinemia is one of the most overlooked drivers of weight gain and metabolic challenges. It is a condition where the body produces too much insulin, often for years, long before blood sugar becomes elevated. High insulin levels increase hunger, promote fat storage, and make it unusually hard to lose weight even with strict dieting or exercise. Many people live with hyperinsulinemia without knowing it, because routine blood tests do not check insulin directly.
GLP 1 medications such as semaglutide and tirzepatide have become powerful tools for treating obesity and insulin resistance. One of the most important reasons they work so well for people with hyperinsulinemia is that they help the body reduce unnecessary insulin production. When insulin levels fall, appetite becomes calmer, blood sugar becomes more stable, cravings decrease, and the metabolism begins to shift away from constant fat storage.
This article explains what hyperinsulinemia is, how it develops, how GLP 1s lower insulin, and why this creates an ideal environment for weight loss. You will also learn how symptoms change once insulin stabilizes, what clinical studies show, and how to know if this approach may be right for you.
If you want to know whether GLP 1 treatment fits your metabolism and health goals, you can check your eligibility here.
What Hyperinsulinemia Is and Why It Matters
Hyperinsulinemia means that the pancreas is producing more insulin than the body needs. Insulin is a hormone that allows the body to use or store energy from food. When insulin is high, the body shifts into storage mode. It becomes difficult to burn fat for energy, hunger signals intensify, and cravings increase.
People with hyperinsulinemia often describe feeling hungry shortly after meals, feeling shaky between meals, or craving carbohydrates more intensely. Over time the body becomes less responsive to insulin, a condition known as insulin resistance. To compensate, the pancreas produces even more insulin, creating a cycle that makes weight loss extremely difficult.

How Hyperinsulinemia Affects Weight
High insulin levels directly influence weight through several pathways. Insulin increases hunger by stimulating ghrelin, the hormone that drives appetite. It also reduces the body’s ability to burn fat for fuel, which makes calorie deficits feel more draining. People with hyperinsulinemia often describe hitting weight loss plateaus early or gaining weight back very quickly after dieting.
The body’s constant insulin production also raises inflammation, increases water retention, and can cause rapid swings in blood sugar that lead to cravings, irritability, or fatigue. These swings can make healthy eating feel harder than it should be.
This is why many people feel like they are fighting their biology rather than simply their habits. Hyperinsulinemia makes the appetite louder and the metabolism slower. GLP-1 medications help reverse this.
How GLP-1 Medications Lower Insulin Levels
GLP-1 medications reduce insulin secretion in a controlled and natural way. They do not shut insulin off. Instead, they help the body release insulin only when appropriate and at more stable levels. This makes blood sugar steadier and reduces the large insulin bursts that drive hunger and fat storage.
Semaglutide, tirzepatide, and other GLP 1s work by slowing digestion, calming appetite hormones, stabilizing glucose, and reducing the spikes that trigger excessive insulin release. Over time this helps the pancreas rest and reduces the hormonal noise that drives overeating. As researchers look to refine this process even further, new non-peptide medications like orforglipron are being developed to target these same metabolic pathways in a convenient daily pill.
Why Lowering Insulin Supports Weight Loss
When insulin levels fall, the body stops storing energy constantly and begins burning stored fat more efficiently. Appetite becomes quieter. Cravings lessen. People feel satisfied with smaller meals. Blood sugar stays steady rather than crashing. The combination reduces the emotional and physical drivers of overeating.
Lower insulin also improves resting metabolic rate. Research shows that people who reduce insulin levels early in weight loss maintain more lean mass and experience fewer weight loss plateaus because their metabolic adaptation is less severe. This means the body does not panic or slow down as dramatically when calories decrease.
Most importantly, when insulin resistance improves, the body becomes more flexible in how it uses energy. This flexibility makes long term weight maintenance more achievable.
What Studies Show About GLP-1s and Insulin Levels
Several studies demonstrate that GLP 1 medications significantly improve insulin resistance, hyperinsulinemia, and overall metabolic health.
A 2021 semaglutide study published in The Lancet followed people with obesity and elevated insulin levels. Participants saw large reductions in fasting insulin, improved HOMA IR (a measure of insulin resistance), and meaningful weight loss. People with the highest baseline insulin levels often experienced the greatest improvements.
Another trial evaluating tirzepatide found even stronger reductions in insulin and C peptide levels. Participants showed improved glucose control, better insulin sensitivity, and substantial reductions in visceral fat. Visceral fat is strongly linked with hyperinsulinemia, so this reduction is a key part of long term metabolic improvement.
A third study in metabolic syndrome demonstrated that lowering insulin levels resulted in significant improvements in inflammation markers and liver function. Given the link between hyperinsulinemia and fatty liver disease, this is a notable benefit.
Together, these studies show that GLP 1s do more than reduce appetite. They actively reshape the metabolic environment that makes weight loss difficult in the first place.
How Symptoms Change When Insulin Improves
People with hyperinsulinemia often feel the effects of GLP 1 treatment quickly. Many describe fewer cravings, more stable energy, and a sense of calmness around food. Others notice they can go longer between meals without feeling shaky or irritable. Afternoon fatigue often improves.
Appetite becomes predictable instead of chaotic. People notice they feel satisfied without large portions. The emotional drive to eat decreases because the hormonal pressure behind those urges weakens.
These changes reflect a deeper improvement in insulin sensitivity. When the body is no longer fighting against high insulin, weight loss feels more natural and sustainable.
Who Benefits Most From GLP-1 Treatment
GLP 1 medications may be especially helpful for people who have symptoms of hyperinsulinemia such as fatigue after meals, intense carb cravings, difficulty losing weight, weight gain around the abdomen, irregular blood sugar swings, or family history of type 2 diabetes.
People with PCOS, metabolic syndrome, or insulin resistant obesity often respond particularly well because GLP 1s target the core hormonal pathways involved in their symptoms.
Anyone who has tried dieting repeatedly without success, despite eating well and exercising, may also benefit. Often the barrier is hormonal, not behavioral.
If you want to see whether your symptoms match hyperinsulinemia or insulin resistance, you can start by checking your eligibility here.
How Lifestyle Interacts With GLP-1 Treatment
Lowering insulin through GLP 1 therapy works best when paired with steady protein intake, high fiber foods, hydration, and gentle movement. These choices further support insulin sensitivity and help preserve muscle mass. Strength training and balanced meals contribute to long term metabolic health and reduce weight regain risk.
As GLP 1 therapy reduces cravings, many people find it easier to make food choices that align with their goals. This creates a self reinforcing cycle where improved appetite control supports better nutrition, which supports better insulin sensitivity, which supports easier weight loss.
What Symptoms Require Attention
Most insulin related improvements feel positive. However, if blood sugar becomes too low, symptoms like dizziness, shakiness, or sweating can occur. This is rare in people without diabetes but should be evaluated if it happens. Persistent nausea, constipation, or intense fullness may also require dose adjustments.
Severe or persistent abdominal pain, vomiting, or inability to tolerate fluids should be discussed with a clinician. These symptoms are uncommon but require evaluation.
FAQs
Does high insulin make it harder to lose weight?
Yes. High insulin drives fat storage and increases hunger, which makes weight loss difficult.
Do GLP 1s lower insulin?
GLP 1s reduce excessive insulin release and improve insulin sensitivity.
How fast do insulin levels improve?
Many people see improvements within the first eight to twelve weeks.
Can I have hyperinsulinemia with normal blood sugar?
Yes. High insulin often appears years before high glucose.
Do GLP 1s cure hyperinsulinemia?
They help reduce insulin resistance, but long term outcomes depend on lifestyle and metabolic health.
Check Your Eligibility
If you want to learn whether GLP 1 treatment or compounded semaglutide is an option for your hyperinsulinemia, cravings, or metabolic symptoms, you can begin with Mochi’s eligibility questionnaire. It takes only a few minutes and provides personalized guidance based on your health history and goals. Check your eligibility here.
References
Jastreboff, A. M., et al. (2022). Tirzepatide once weekly for the treatment of obesity. New England Journal of Medicine, 387, 205 to 216.
Kahal, H., et al. (2021). Hyperinsulinemia and metabolic disease. Diabetologia, 64, 994 to 1007.
Lundgren, J. R., et al. (2021). Healthy weight loss maintenance with semaglutide. The Lancet, 397, 971 to 984.
Meier, J. J. (2020). GLP 1 receptor agonists and insulin dynamics. Journal of Endocrinology, 246, R57 to R75.
Sanyal, A. J., et al. (2019). Insulin resistance, NASH, and metabolic syndrome. Hepatology, 70, 137 to 149.
Thomas, D. D., Corkey, B. E., Istfan, N. W., & Apovian, C. M. (2019). Hyperinsulinemia: An early indicator of metabolic dysfunction. Journal of the Endocrine Society, 3(9), 1727 to 1747. https://doi.org/10.1210/js.2019-00065
Read next
Ready to transform your health?
Unlock access to expert guidance and a weight care plan crafted just for you.

Ready to transform your health?
Unlock access to expert guidance and a weight care plan crafted just for you.

Ready to transform your health?
Unlock access to expert guidance and a weight care plan crafted just for you.


© 2026 Mochi Health
All professional medical services are provided by licensed physicians and clinicians affiliated with independently owned and operated professional practices. Mochi Health Corp. provides administrative and technology services to affiliated medical practices it supports, and does not provide any professional medical services itself.


© 2026 Mochi Health
All professional medical services are provided by licensed physicians and clinicians affiliated with independently owned and operated professional practices. Mochi Health Corp. provides administrative and technology services to affiliated medical practices it supports, and does not provide any professional medical services itself.


© 2026 Mochi Health
All professional medical services are provided by licensed physicians and clinicians affiliated with independently owned and operated professional practices. Mochi Health Corp. provides administrative and technology services to affiliated medical practices it supports, and does not provide any professional medical services itself.

















